The coronavirus pandemic continues to be a disruptive force for patients and physicians across the US, creating a domino effect with catastrophic consequences. Beyond the wave of patients infected with COVID-19, healthcare systems are also experiencing drop-off from non-infected patients who have had to adjust their healthcare utilization habits. A decrease in prescription adherence, delayed diagnoses and lack of physician visits are just a few of the detrimental side effects of “physician distancing” that are now common among US patients who are not in the COVID-19 infected population.
These effects are increasing the risk of further hospitalizations at a time when US hospitals are nearing full capacity. Thousands of patients are being asked to postpone or cancel their much-needed surgeries and treatments due to either overcrowding or a life-threatening lack of protective materials at hospitals. Even for patients who aren’t being instructed to stay home, many are forgoing therapies, presumably out of precaution. “The most concerning possible explanation is that people stay home and suffer rather than risk coming to the hospital and getting infected with coronavirus,” reports Harlan M. Krumholz, M.D. in a New York Times article entitled Where Have All the Heart Attacks Gone? “This theory suggests that COVID-19 has instilled fear of face-to-face medical care.”
To track the drop-off (and eventual uptick) of patients visiting their doctors and/or switching to telehealth visits, HealthVerity has created the HealthVerity Patient Confidence Index (HVPCI).
What is the HVPCI?
The HVPCI is the first of its kind—it represents a measure of physician visits by non-COVID-19 patients across 20 key therapeutic areas. It indicates the bi-weekly change of patients visiting their doctors and specifically highlights the sharp decline in visits since the coronavirus pandemic took hold in the US in early March. The index helps track how patients are responding to a broader awareness of COVID-19 as well as guidance from public health officials. By measuring real-world visits, it serves as a crucial expression of the confidence in patients to seek care for acute and chronic illnesses in the healthcare system.
As coronavirus cases peak and eventually subside in the coming months, this indicator will continue to serve as an overall measure of US patient engagement. With each future release of the HVPCI, the level that patients are re-engaging with the healthcare ecosystem, down to the specialty, is revealed.
The 20 key therapeutics areas represented:
|
|
This week, HealthVerity reported the first national benchmark score of 68, indexed against a pre-pandemic score of 100 for patient confidence. The score compares the current number of in-person doctor’s visits to the number this time last year. The current score is considered “critical” in terms of patient engagement with the US healthcare system. A critical score signals the overwhelming reluctance by patients to visit their physicians for treatment. The trend is directly contributing to challenges in adherence and access to chronic medications, especially injectables and infusions, and a decline in first diagnosis for many important diseases.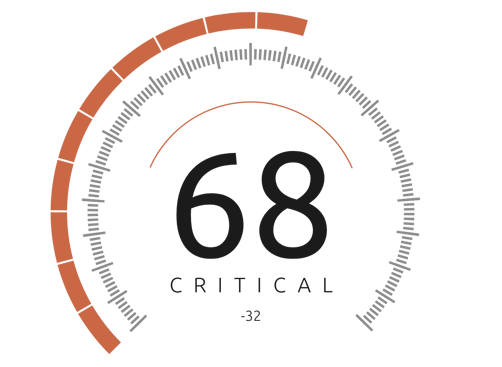 The longer these patients wait to seek treatment, the more dangerous their conditions can become. In an article for ProPublica, Joanne Lipman writes, “Those ripple effects are only just starting to be felt. If we aren’t vigilant in taming the COVID-19 crisis... we’ll have another crisis in the making. Flattening the curve is indeed essential to save lives—and not just those of COVID-19 victims.”
The longer these patients wait to seek treatment, the more dangerous their conditions can become. In an article for ProPublica, Joanne Lipman writes, “Those ripple effects are only just starting to be felt. If we aren’t vigilant in taming the COVID-19 crisis... we’ll have another crisis in the making. Flattening the curve is indeed essential to save lives—and not just those of COVID-19 victims.”
Tracking trends in patient utilization with the HVPCI not only has the power to save lives, but it’s also one of the best ways to investigate or test certain hypotheses surfacing in the market around the impact of COVID-19.
Critical findings from the HVPCI
The first reported measure from the HVPCI indicates that the most impacted specialties, as measured by weekly medical claims received, include ophthalmology, dermatology, otolaryngology, endocrinology and rheumatology. Specialties such as surgery, cardiology and oncology are also experiencing declines consistent with the broader market. Not surprisingly, the least impacted discipline was infectious disease, which still scored below the baseline score of 100.
Increase in telehealth visits
As a further indicator of the dramatic shift in patient behavior since the arrival of COVID-19 in the US, the top 20 physician specialties have seen an exponential increase in telehealth visits. Data supporting the development of the HVPCI indicates a ramp in telehealth of 1,090% in the past 30 days, with the largest demand for primary care, pediatrics, behavioral health, cardiology and gastroenterology.
Many health plans and hospital systems encouraged telehealth visits by waiving co-pays and creating on-demand scheduling. While telehealth represents less than 8.0% of the total claims received, the trend is expected to be an important equalizer with respect to near-term physician distancing. According to recent predictions by Forrester Research, telehealth visits are expected to surpass one billion in 2020. This new projection includes 900 million visits related to COVID-19, 200 million general care visits and 80 million visits related to mental health needs. The same article adds: “We anticipate a spike during the pandemic as citizens grapple at home with the stress and anxiety that come with a period of uncertainty.”
As patients are unable to access care in a safe manner, the potential for even more hospitalizations grows on a daily basis. The HVPCI is positioned to measure the recovery of the US in the coming months and the confidence that patients have in re-engaging with the healthcare system. Health organizations, life sciences companies, insurance providers and additional organizations looking to better understand the results of this pandemic on the population as a whole can now leverage these details to adapt and prepare for the inevitable fluctuations in healthcare and beyond.
“HealthVerity is well-positioned at the center of the largest, fully interoperable data ecosystem in the US, and we proudly present the HealthVerity Patient Confidence Index as a stark reminder that there are two sides to the COVID-19 story,” said Andrew Goldberg, chief operating officer of HealthVerity, in a recent press release. “We expect the HVPCI to enable pharma, insurers and key authorities to keep the long-term focus on restoring the confidence in our country’s national provider network and to enable patients to safely seek the care that they need.”
To learn more about HealthVerity’s efforts to educate and inform on COVID-19, please visit our website.





